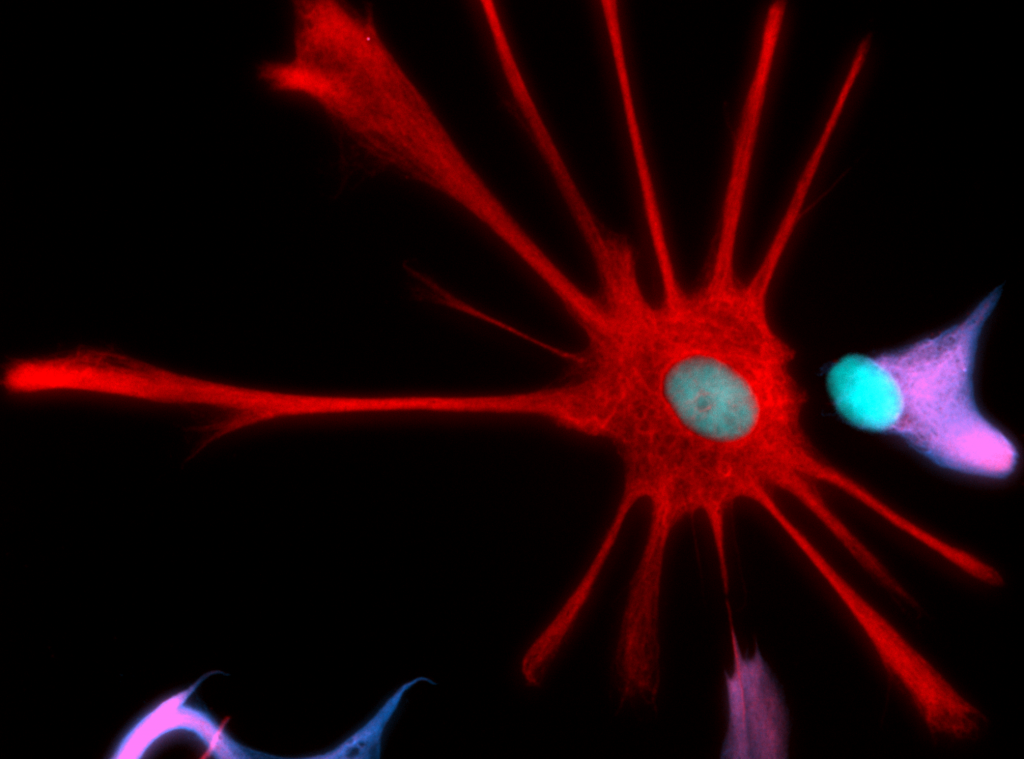
What is “ALS In a Dish?”
When a 2008 collaboration between the Project ALS/Jenifer Estess Laboratory for Stem Cell Research, the Henderson and Wichterle labs at Columbia, and the Eggan lab at Harvard, yielded the first patient-derived cellular models of ALS—ALS in a Dish, as we affectionally called it—many researchers believed that better ALS treatments were right around the corner. For the first time, scientists were able to make an unlimited supply of motor neurons from actual ALS patients, and use these cells like a cancer researcher uses cells from a patient biopsy—to understand what is going wrong in a specific ALS patient’s motor neurons, and easily screen thousands of drugs to find which ones correct the problem. ALS in a Dish was swiftly and widely adopted by the ALS research community and lauded by Time magazine as their scientific breakthrough of the year.
[Sidebar: What is ALS in a Dish? Diagram with explanation of “induced pluripotent stem cell” model]
It’s not hard to spot a problem here: it’s been more than ten years since this ALS in a Dish model was developed, and there are still no meaningful treatments available for people with ALS. Of course drug development is slow—but the truth is that even as this breakthrough model has been adopted for drug screening by hundreds of academic researchers and even drug companies around the world, several issues have prevented ALS in a Dish from living up to its name and reaching its potential gold standard status for ALS drug screening. To name a few:
- ALS in a Dish doesn’t look like ALS in a person. The most critical problem in using iPS-derived motor neurons to screen drugs is that—even though they were developed from a person with ALS, whose motor neurons are going awry—they just don’t get that sick on their own. While researchers aren’t sure why, one common hypothesis is that the ALS in a Dish motor neurons are just too young to develop ALS on their own. Regardless of why it happens, it’s hard to effectively screen drugs for ALS on motor neurons that don’t look that different from healthy motor neurons.
- ALS in a Dish looks different depending on who makes it. There are many cooks in the ALS in a Dish kitchen, and unfortunately, they’re all using different ingredients and recipes, then wondering why their final dishes don’t look alike. This lack of standardization is a problem for researchers using the ALS in a Dish model, who often report different results from what should be the same disease model—disturbingly, even in cases when the cells came from the exact same patient.
- ALS in a Dish is ultra-sensitive to environmental and genetic differences. When Project ALS researchers first tested drugs on ALS in a Dish, we used iPS-derived motor neurons from healthy people as the “healthy motor neuron” counterpart in these studies—but over the years, we’ve learned that even among so-called “healthy” motor neurons, there’s a huge amount of variability in the dish. Researchers have also learned that there can be wide variability even between people with the same genetic form of ALS, and that the same ALS in a Dish can look very different with even tiny changes in timing, temperature, or location of an experiment. Minimizing this background noise is essential to getting reliable experimental read-out.
Project ALS has believed in the promise of stem cell models of ALS since we got to work more than 20 years ago, and Core researchers—led by the same people who developed ALS in a Dish 10 years ago—are taking big steps toward improving this currently useful model toward its transformative potential. At the Core’s in vitro screening unit, we’re taking two parallel approaches to maximizing this model’s utility for drug screening:
- To screen drugs now, we use chemicals that mimic ALS to make iPS-derived ALS motor neurons to get sick faster. We use a chemical called cyclopiazonic acid (CPA) that causes our ALS in a Dish model to accumulate the gunked-up, misfolded protein seen in ALS patients’ motor neurons. Then, we screen thousands of potential ALS therapies against this chemically induced model of ALS and identify which drugs save ALS motor neurons. Core researchers have now expanded this model with different chemical stressors that mimic other key biological stressors in ALS.
- In the meantime, leading stem cell biologists at the Core have collaborated with experts in new genetic technologies to develop a next-generation ALS in a Dish screening platform. This new approach, which we’re now validating in-house and will be using for future drug screens, allows us to put iPS-derived motor neurons from multiple patients in the same dish, tag each one with a genetic barcode, and test drugs on dozens of cell lines at the same time. This new system will allow us to accelerate our drug screening, and to really evaluate whether the differences seen in different genetic backgrounds for ALS in a Dish mean that there are many “flavors” of ALS, or are just anomalies from each researcher’s different procedures and lab environments.
[Sidebar: The Core’s approach – diagram showing first-gen and next-gen approaches]
Example only – to be updated
The Core’s mission is to deliver better drugs to people with ALS, and ALS in a Dish is an important tool toward rational drug discovery and assessment. We are excited by the therapeutic compounds this model has yielded so far, including our lead drug candidate PHB [link to PHB post], and we are excited to apply our next-generation model to identifying better drugs for specific ALS patient types. Through the Core, we aim to realize the ALS in a Dish model’s potential as the gold standard for highly efficient, accurate, patient-specific drug screening toward better ALS drugs.
Further reading:
https://www.frontiersin.org/articles/10.3389/fnins.2017.00671/full